Trigger Warning: Hospital details, death, Charlie’s final days. Photos – happy and hard ones. It’s amazing what you will take photos of when it’s the last photos you will get to take of your child. I didn’t share the most painful ones.
We have a diagnosis now officially for Charlie confirming Leigh’s disease. I have been waiting to tell the story until we knew for sure what it was. This blog tells about our journey through Charlie’s life to where we are now. Some of it positive some of it hard. It talks about what we saw but what was also common in toddlers so shows how we didn’t know this was coming. There is my very vivid memory of our last day with Charlie and it’s very difficult. You can choose to skip to the end where I talk more about the diagnosis or go along for the journey
If you knew Charlie you knew earlier in his life he was very clingy and snuggly. I didn’t mind. He would have breath holding spells, had trouble nursing for long enough periods of time, so we were substituting with formula. He had some reflux issues, constipation and weird noises sometimes when he’d breathe that they told us was from under developed vocal cords due to arriving early at 37 weeks. His eyes would bounce back and forth quickly when he’d focus sometimes. We did take him to a paediatrician for his breath holding spells. He told us he’s just an angry baby and it’s a sign of temperament and we would just have to teach him that’s not how to handle anger. That didn’t sit right with us because often times Charlie seemed scared when it happened. We had also read that science has shown it’s not got anything to do with temperament as it wasn’t intentional. Our family doctor at the time had hoped he would assess for seizures because my aunt had absence seizures as a kid and Riley had been watched for it and assessed because we thought she was having them. (now we think it was a coping mechanism for anxiety and not seizures for her). He also reviewed our family history and told us anxiety is not a thing. So our doctor didn’t like that either. Charlie continued to grow and develop so we moved on.

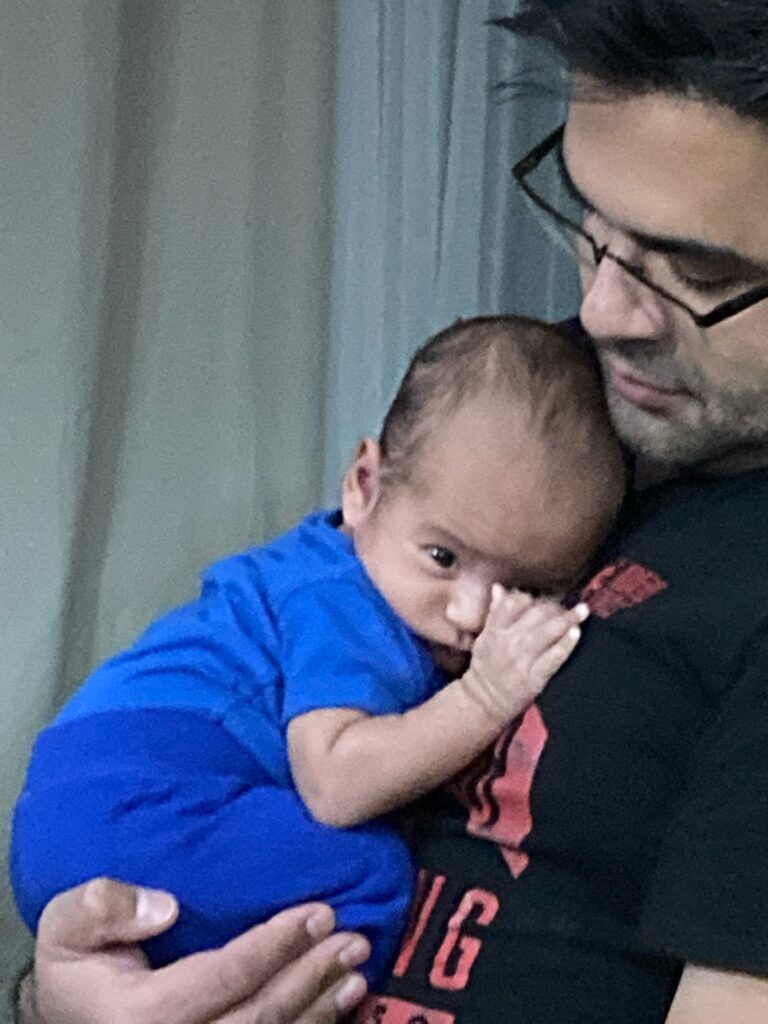
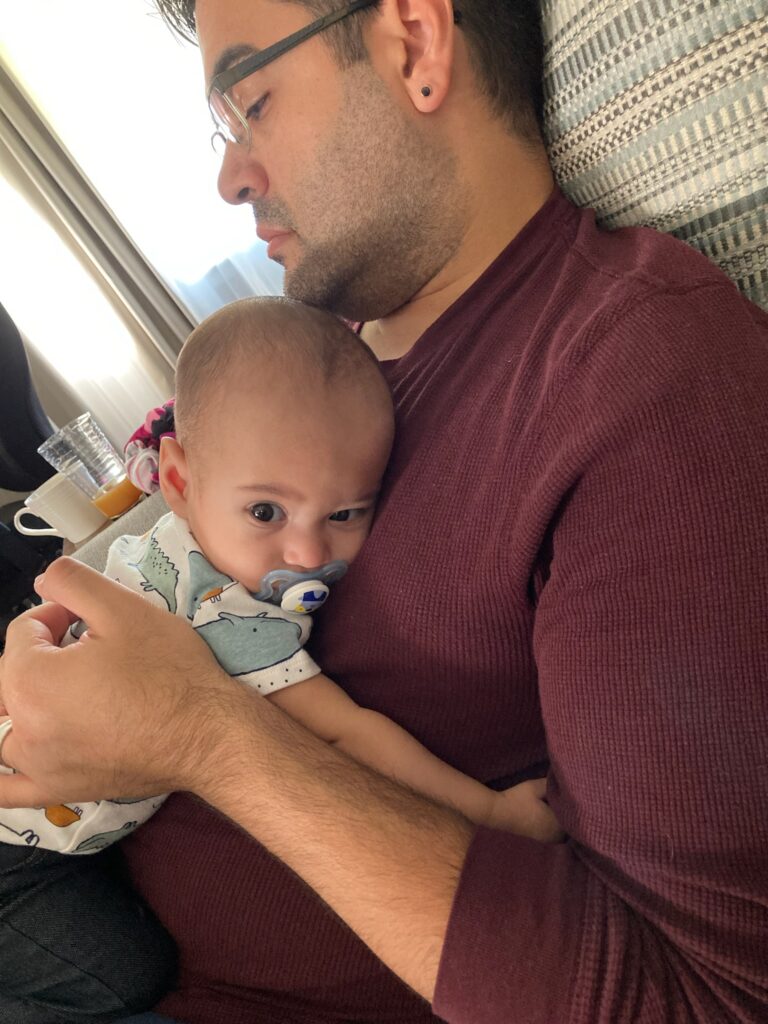





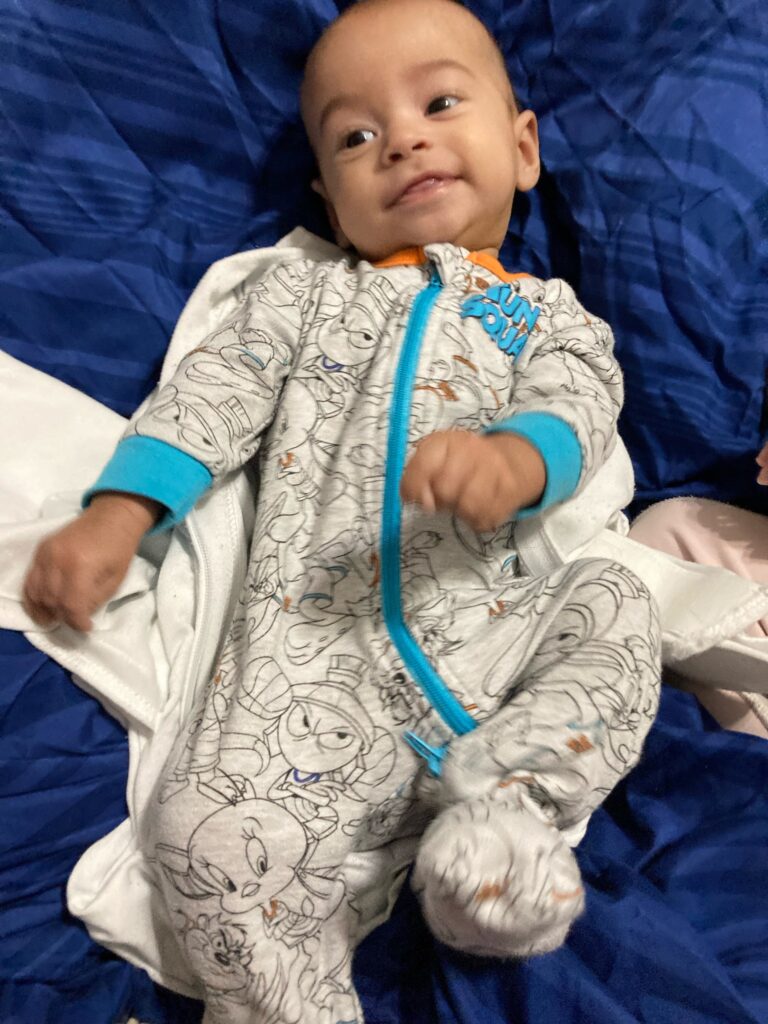
In theory though he was happy. All of these things are normal things that happen to healthy babies. He was meeting his milestones on time. I had to remind myself sometimes that Riley was early so it was okay that he hadn’t met them yet because he wasn’t expected to. and then he would get it by the time he was supposed to.




Until that stopped. Shortly before his 15 month appointment I wondered if his weight had slowed. The appointment though went well there wasn’t enough of a slow down to cause concern. He sort of had his 5 words -Dadda, Nana (which we think was his name for me) duh – for the dog Dusty, der or wa- for water and good. At this point he was walking with support. Which he had been doing since around 12 months. He kind of waved. and kind of high fived. He definitely pointed. Sometimes too we were starting to think he was saying Rala for Riley. He had all kinds of consonant sounds and combinations of them gl was one I remember him using.
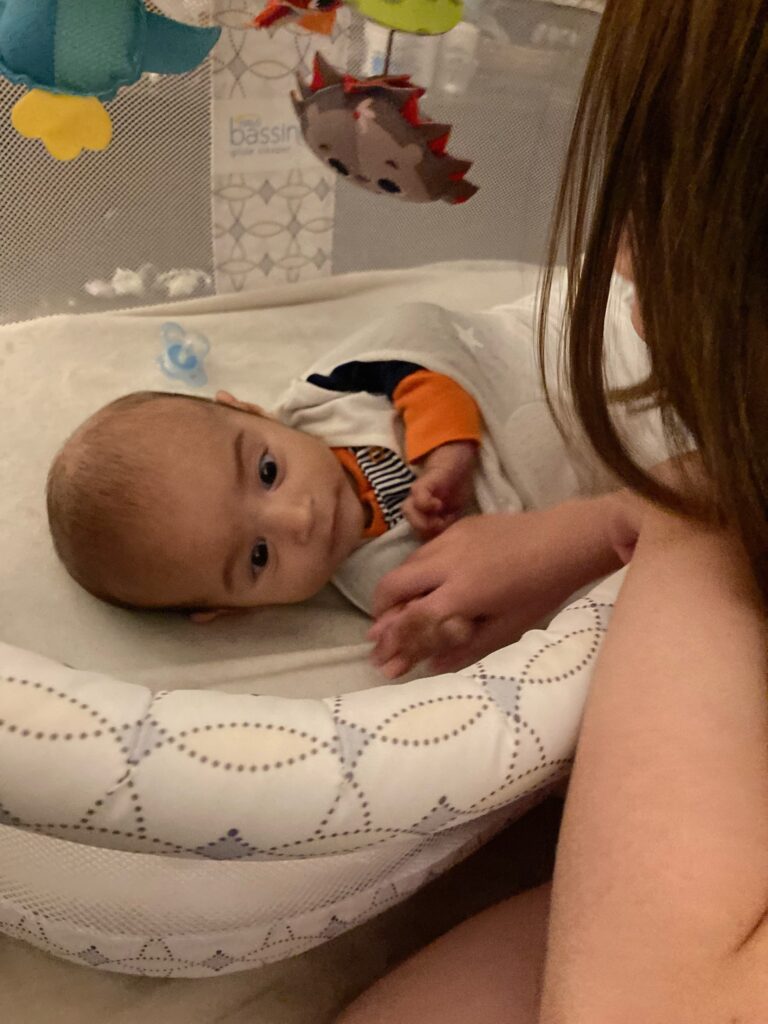
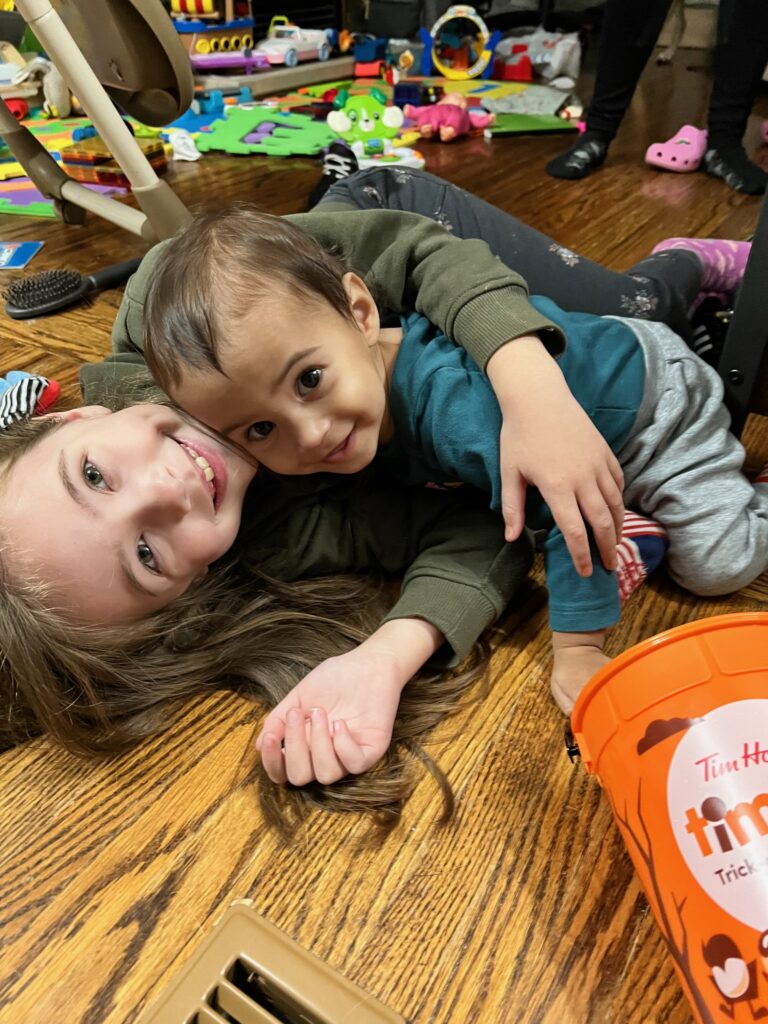
Around 16 months I started noticing his belly looking wrinkled like loose skin after someone lost weight. He wasn’t really saying his words any more just making lots of sounds and gestures. And he still couldn’t walk without support. I was really concerned though about the weight. When Ivars noticed the loose skin and that he was starting to see his clothing looking bigger he agreed something wasn’t right so we went back to the doctor. Early in his life our doctor was transitioning in things in her life going on an emergency medical leave and eventually leaving the practice. So we kind of kept seeing different people. At this point the locum doctor had now seen us twice and was in agreement something wasn’t right. She put referrals in for paediatricians all over and got us into the dietitian in her clinic. Life continued but with more frequent check ups with the new doctor. Charlie was a sleepy baby but that was fine by me because I’m a sleepy mommy. He loved being outside though. It made him so happy to just even go for a ride in his stroller or the wagon. He loved to people watch. Loved the swings. He was in a music class but it was in the morning during his nap time and in retrospect when things started happening so he was often tired and not all that interested. But at night he came alive. He was super playful scooting around to see Riley in her room, playing with his cars and his boat. Banging on things and making noise with whatever items he could.Playing in the toy kitchen. Sitting outside Riley’s room while we tucked her in for the night. He loved books. He didn’t really sit still for you to actually read it fully though because he really liked turning the pages himself and looking closely at the pictures and feeling the textures of the pages. We put a tiny little shelf on the wall that held a few books by his play area so he could get to them. He’d crawl over and pull himself up on a toy work bench or reach for help to stand and grab a book then sit down and “read” it.


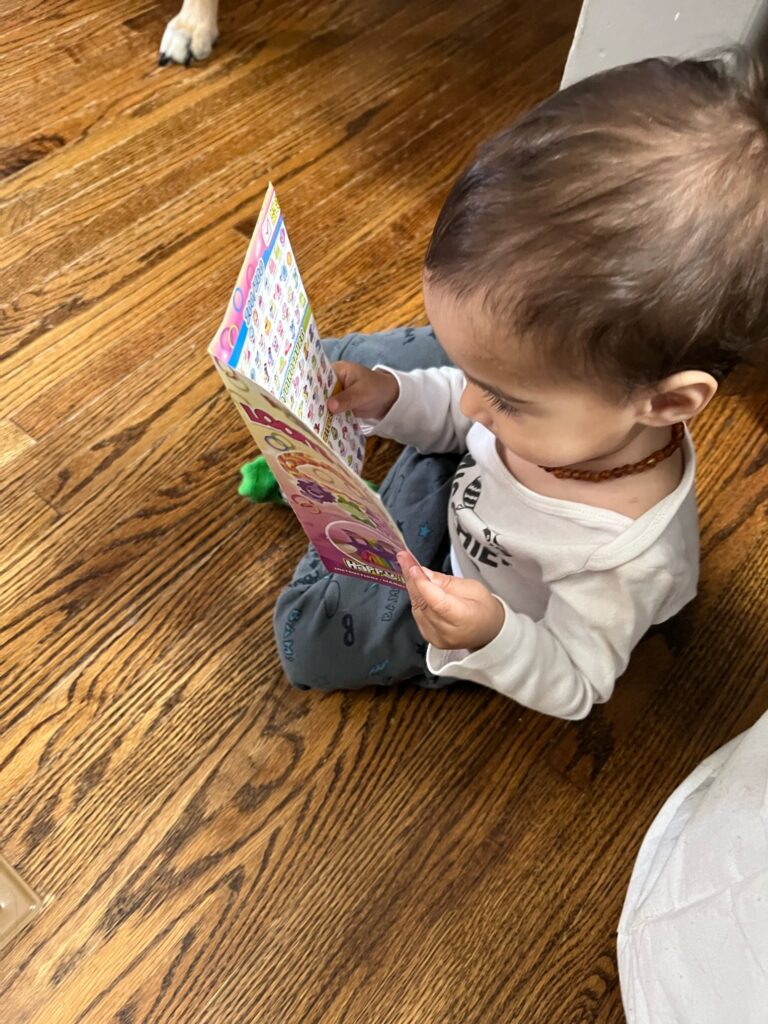







As time went on we waited and waited for the paeds. Charlie was definitely losing weight and had definitely lost his words now and by 18 months (December 2022) still was not walking without support. He wasn’t really meeting any of his 18 month milestones either. He was having issues with foods of different textures and was getting really picky about what he ate. He seemed to understand everything going on around him but couldn’t really say anything.
Christmas Eve we got together with the extended family seeing all my cousins including cousin and ER nurse Ted (name changed for privacy). We had briefly told Ted some stuff was going on and we had referrals in. A few weeks later, just a few days after New Years I texted Ted. I was getting frustrated and really worried that no one was taking Charlie on and I was getting concerned because he didn’t seem to be eating as much as well. Ted admitted she was also worried by how small he was. She suggested it might be time to bring him to the ER and let them intervene because it would get the paeds involved sooner as well as other care he was probably going to need. Ivars wanted to wait until we had an appointment with the dietitian that was scheduled for that week before we did. So we went to the appointment. She offered some suggestions and we went home hopeful they might work. Within the next week two paediatrician offices called having accepted the referral. We actually at the time weren’t sure if one or the other specialized in anything so we took both appointments. At the family doctor check up that week she said she had planned on sending us to the ER until she heard we got accepted. She had spent the holidays calling other offices herself and sending letters notifying them that Charlie had reached the point of a Failure to Thrive diagnosis.
The first one we went to didn’t sit quite right with us he seemed to feel that Charlie’s biggest problem was constipation and that solving that would solve everything. He wasn’t bad but didn’t seem as thorough as we felt Charlie needed. The second one. Dr. Gambarotto was amazing though. Her office had called and said that Dr. Gambarotto wasn’t taking any new patients but felt Charlie’s information indicated it was an emergency. We came in and she told us she was extremely concerned seeing his notes. She immediately got referrals for everything going letting us know a lot of things are a long wait so better to have all the referrals in and cancel it if we don’t need it then wait until it’s too late. She got us an in home Occupational Therapist and an in home Dietitian. Referrals were in to speech therapy, physiotherapy, an ENT, and more (not neurology though at this point).
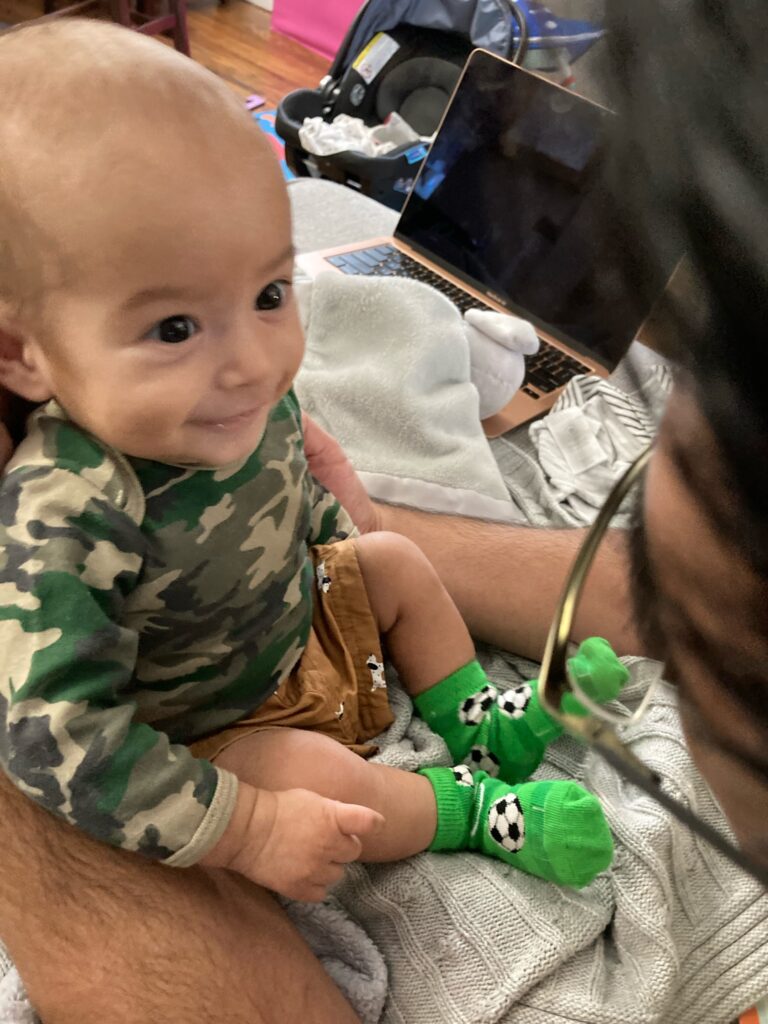
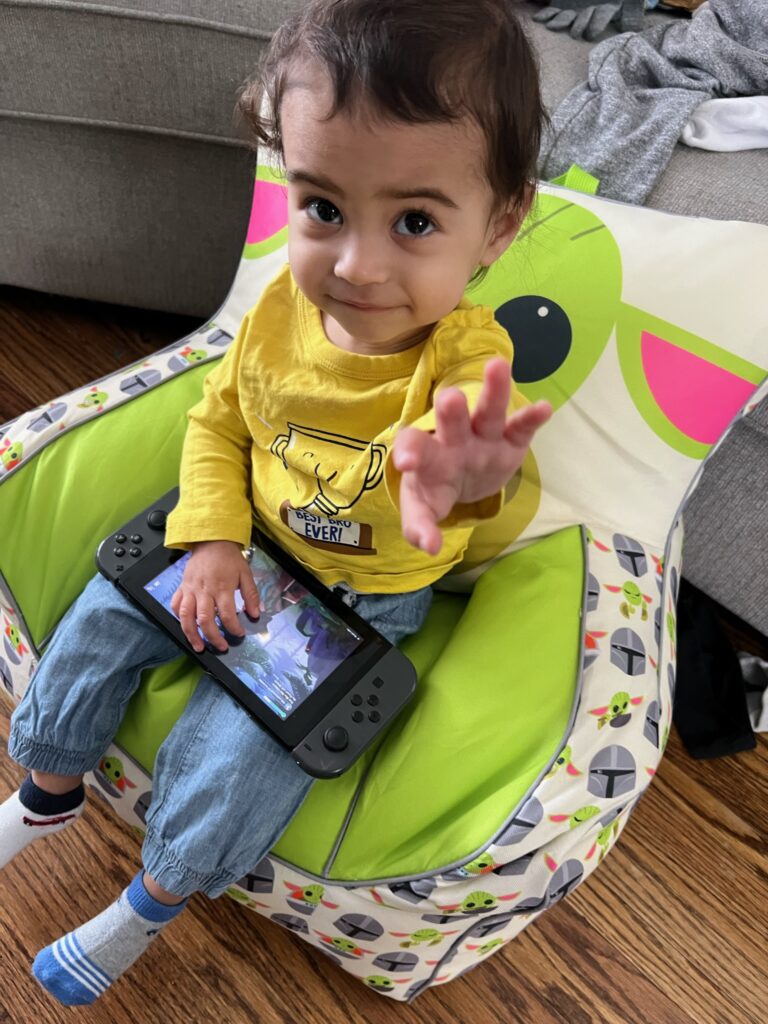
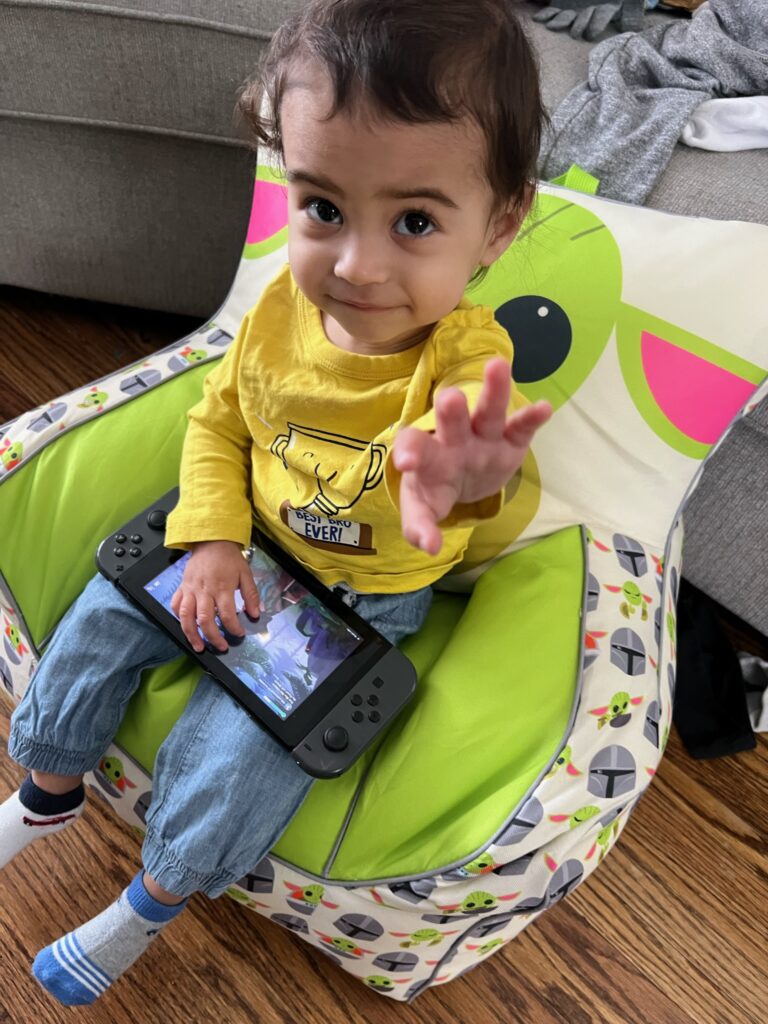
He was actually still happy and playful through all this time though. His interest in play and independent play was really progressing and he had got many musical instruments for Christmas that he recognized from music class and was really happy about. He really loved them. He had watched Ivars and Riley and I play video games and had a toy controller. But he didn’t want the toy one he wanted ours and one day he sat down and held up the switch controller to the screen and pressed a button. The game turned on and he squealed in excitement. He was then making the character walk around. He was so smart. This became something he loved to do.
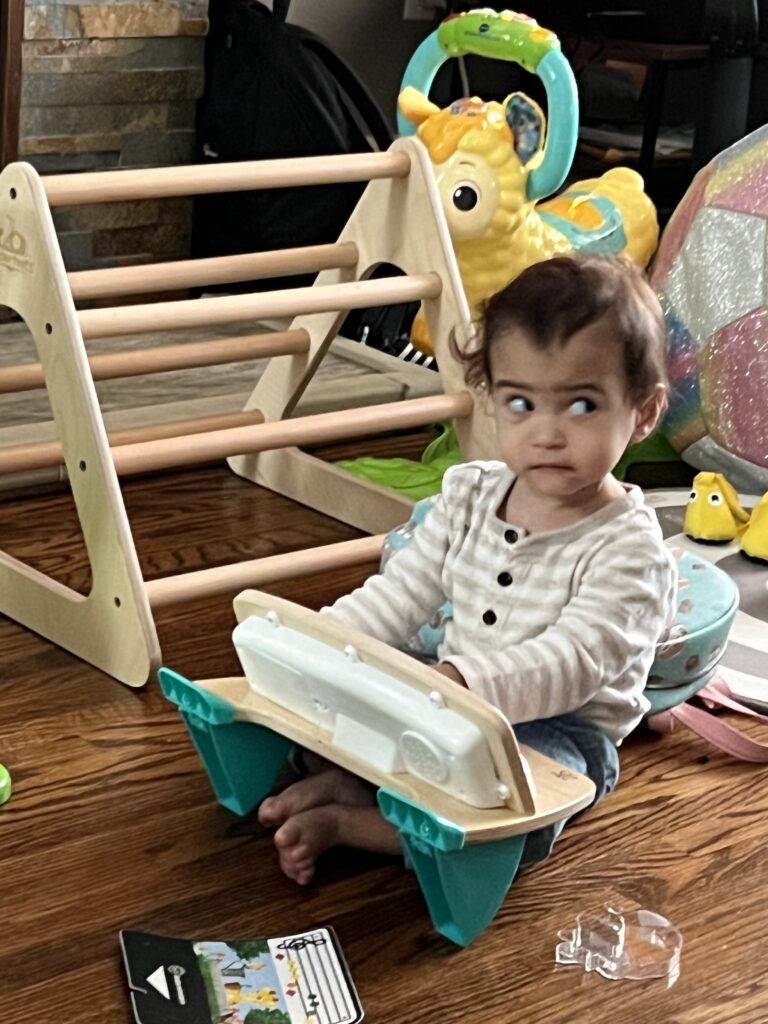








Eventually working with the dietitian and the OT we made some changes. We moved Charlie from a high chair to a booster seat that gave him better sitting support and an easier reach of things. The OT noted he used a lot of energy eating so these changes helped make it easier on him increasing his appetite. We were basically told whatever he will eat let him eat even in copious amounts. Thats when chocolate panettone, McDonalds nuggets and fries and corn twists became staples. The dietitian also directed us to a powder that could be added to his formula to increase calories. Charlie began gaining weight. He started making developmental improvements as well, learning how to sit and climb on chairs and furniture and how to put his leg over a ride on toy to sit on it. He had new sounds to communicate with us and we THOUGHT that was a good thing because he had figured out ways to let us know things. However, we didn’t realize as this was happening he was losing his consonant sounds.
End of February Riley and I caught COVID. Somehow Ivars and Charlie were fine. Charlie did seem more tired but he also began fighting that second nap. He started daycare at then end of February two days a week but he wouldn’t eat while he was there. Because of his weight we couldn’t afford that so we picked him up after lunch and fed him at home. Dr. Gambarotto saw him just before he started daycare on his own. (We started slow because of his development we wanted to see how he did so we would go and stay with him or stay in the building at first) She was thrilled with his development and weight gain. He gained so much she said even a healthy kid doesn’t gain that much in a short period. She agreed though that if he wouldn’t eat at daycare we were going to need to make sure he came home to eat. We’d send him with his own favourite foods and he’d sit with the kids in hopes he’d start eating with them and we’d pick him up before they napped.
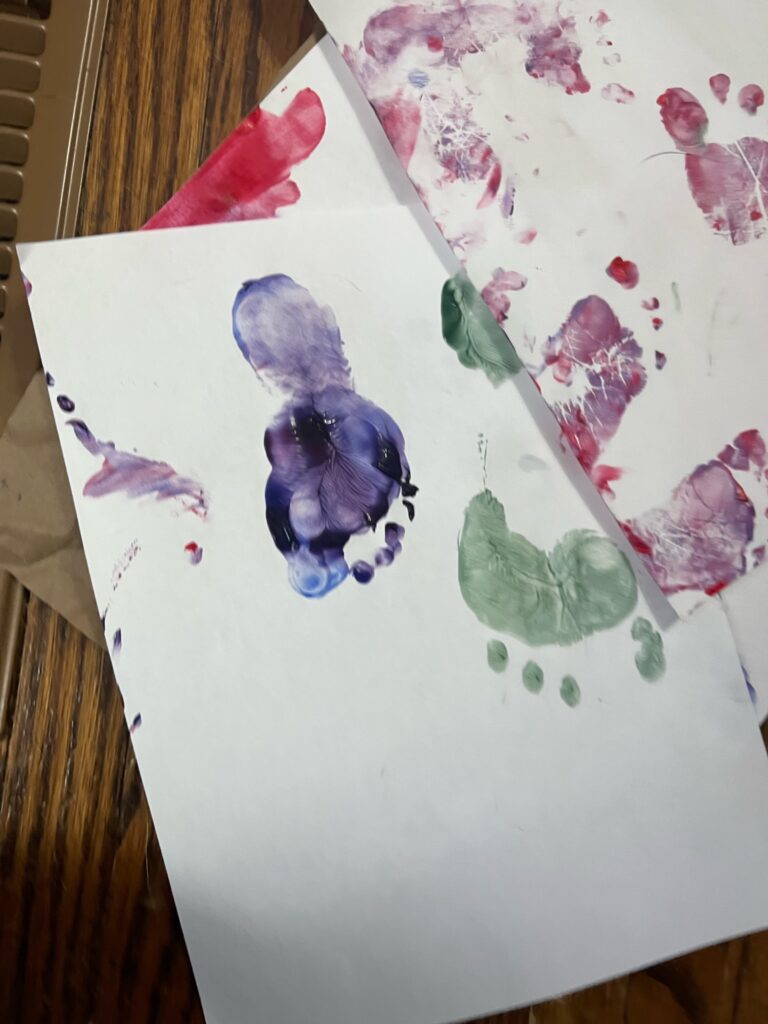
Daycare was good too. The resource teacher gave some tips as well on how to make him more comfortable with textures using playdoh and finger paints etc. thinking it may help with food exposures. We also discovered the idea of using a sensory bin I had been using for him for water play instead because he hated the bath but this way it was in a smaller surface area he could control. He had been to daycare on his own for about a week or two when he got really sick for 3 days. Super lethargic and sleepy, hoarse sounding a bit of a cough. Seemed exactly how he was in May 2022 when he had COVID so we thought he got it too but kept testing negative. Eventually he recovered but couldn’t shake the cough. The doctor prescribed him Ventolin and he got back to daycare for a day. All of sudden the weekend of March 11/12th his cough started sounding worse again. He started sounding wheezy and had gurgles. I was sure it was pneumonia. We woke up the Sunday morning and I was to read at Mass that day but I really didn’t like how Charlie sounded. I booked an appointment at McMaster’s cold and flu clinic for their first appointment. I missed a training meeting I arranged because my gut said something is wrong here. We went to Church but the noises he kept making made me so anxious I couldn’t read and by the end of mass I was in tears. We got him to the hospital. They checked his vitals and listened to him. They prescribed a steroid inhaler. I remember though going into work after because there were classes. When I got there and saw my coworkers I broke down and cried. Something was wrong with my baby I just knew it. There is more here we aren’t seeing. They comforted me but really all his symptoms could have been such every day things so they kinda thought I was seeing things worse than they were.
The puffer seemed to be the answer though. All of sudden Charlie was breathing better and back to daycare. He was playing more with playdoh and starting to actually make marks with crayons on paper and he was finally playing in water I have video on March 28th of this exciting moment. I introduced him that day to MarioKart!
Overnight though that night Charlie woke us up multiple times screaming like he was uncomfortable or in pain. He didn’t seem to be awake though. Riley had a spell of night terrors at his age so this looked very much like them.
Wednesday, April 29th. In the morning while Riley got ready for school and Ivars got ready for work I noticed the noise kind of came back in his breathing and he was really sleepy. I let him sleep until it was time to take Riley to school. On the way home he looked really dopey. I took him in the house and took him to bed. As I laid there I noticed the breathing noise getting worse. Then he fell asleep and a few minutes later her did the screaming thing again followed by like a weird chest noise. Then settled back. I started watching him breathe. Looking for that tell tale sign of respiratory issues the doctors tell you to look for when their stomach sinks in when they breathe in. It didn’t happen but he still sounded weird and so I took some videos to show the doctor sent it to Ivars. I called the doctor and booked an appointment for 2:30 in the afternoon. I woke him up and got him his puffer. He sounded really gurgley too. So I figured it must be mucus and gave him his saline rinse. He pointed to the table which he does when he’s hungry. I sat him down and gave him food but he just stared so blankly it was the scariest emptiest look. “Is he just that tired?” I wondered and took another video. So I took him back to bed hoping the saline rinse and the puffer did the trick. It didn’t and now I was noticing as he lay on his side it kind of sinking in so I took another video then I texted Ivars again and he said “well if you think he needs to go to emergency take him”. I looked over at Dusty our dog who had been staying close and realized he was shaking. Charlie was now awake again but so distant and I was now feeling terrified. I called Ivars and said I’m going. I packed up our things sent the videos to my mom and headed out. The school called saying Riley needed to come home sick with a cough. I thought well the school is on his way he’s fine when he’s upright and awake no cough or weird noise maybe I can stop. As we are driving I’m looking in the mirror and I can see his eyes just looking blankly and like he’s struggling to keep them focused and his head looks unsteady. Voice to text to Ted to see if she’s working ER and let her know I’m taking him down. I called mom at this point freaking out and telling her what’s going on. She sent my videos to Ted and told me my dad coincidentally is on lunch and just left work to head to see my grandma so I called him as I drove past the school and he agreed to pick up Riley. Ted texted me that the breathing coughing ones were hard to say that it was something concerning but his blank look face absolutely was reason to get him there. When I got there I couldn’t find parking and his head started to look wobbly. I think he cry/screamed a little when we went into the parking garage (to be fair he didn’t like parking garages) but I really remember seeing him in the mirror looking like he was going to pass out and starting to think FUCK I should have just parked in front of the fricken hospital doors or called 911. I found the tightest spot next to a pole and a car not parked straight and I’m in the SUV. I took a chance and pulled in. There’s a scratch on the bumper. It could be from the pole but I didn’t hear it and didn’t care. I had to get Charlie out of the opposite side because now I couldn’t open his door. “It’s okay baby I’m getting you help, mama’s going to get you help, this is going to make you feel better okay.” Up the elevator. He hates elevators. Screams and cries all the time. He’s silent now fuck this isn’t good. Run to emergency room 4-5 hour wait time FUCK that’s longer than the doctors office. Still if something bad happens he’s here already. They check me in and the triage nurse brings us in right away. He’s good at his job. He’s friendly and calm. I tell him what I saw this morning. Checks little man’s vitals. Charlie is actually sitting upright on my lap but he’s not really fighting the nurse checking him out. I tell the nurse he hates elevators and he didn’t even seem to notice it on the way up. He looks at his tummy and explains what he’s looking for with his breathing I told him I was watching for that but it’s not happening and I said and he’s awake but he’s like not there. He says “yeah that’s what I noticed too. How’s his colour to you?” “He looks greenish honestly not right” “yeah that’s what I was thinking, I just want to take him to another room to try another machine his oxygen is kinda low so I just want to double check it”. As we walk into the other room I notice the door says resuscitation room. “fuck that’s not good” I think. He starts hooking him up to the monitors. Residents and other nurses start coming in. Definitely not good. “His oxygen is 39%” Wtf I was at 80 something and delirious in the hospital after his birth 39% sounds bad. Residents and doctors and nurses start asking questions. There’s a lot of confusion because he’s not presenting like anyone with 39% blood oxygen. He’s actually still paying attention to what’s going on and he’s actually fighting being put down away from me. They put an oxygen mask on him and he starts fighting. He’s strong enough that they actually want me to hold it and hold his hand. “You are doing so good mom” someone says “you are being so strong it’s hard most parents get really anxious and we need you to help stay calm and your doing amazing” I honestly don’t know who said that. Ivars arrives from Oakville. I’m terrified and I want him standing with me but they’ve got him off in the corner. I’m thinking he needs to be here. Charlie needs to see him. But there’s so many other people and they are all trying to do things. Get him hooked up on things, test his blood. Now they want him to take Ventolin “I’ve already given him 4 puffs it’s not helping” they keep trying they put the Ventolin in the mask and just let it flow. “It’s okay buddy I know it’s scary but I promise this going to help this is going to make you feel better. Daddy is here okay? Daddy and Mommy are here you are going to feel better this is going to help” “You are so good mom” Somewhere now I can feel myself drifting out of my body. I can see the nurses looking at me but I’m disassociating. It felt more like a protective mechanism though. So that I could continue holding his hand and being with him the emotional part of my brain was turning off. I needed Ivars with us, not stuck across the room. I need to stay calm so Charlie here’s my hand I’ve got you baby.
They switch me to the other side now. I can’t really remember why. Now I can see Ivars I feel like my eyes were trying to tell him “our baby is dying we are going to lose our baby”. They tell us they are going to have to intubate him. I think he was sedated at this point. I am slipping into my trance but I’m holding so tight to his hand. I’m standing so strong. but the nurse looks at me. “Mom are you okay?” I nod. “This next part is kind of hard to watch do you need a break” tears start pouring, he needs me but I’m falling away. I need Ivars to stand here. I slowly nod and they slowly pull me away. They suggested it might be hard for Ivars too and that perhaps we should both go get air now. A social worker comes and starts talking to us. She seemed nice but honestly I just wanted Ivars. He was stuck standing still in view of the room. I needed Ted. The social worker gets me water. Ivars lets her know it needs to be ice water. He helps me find my Ativan. I’m still not panicking I’m just missing from myself. The social worker steps back for a bit. I call Kelly to tell her I can’t work tonight and I have a feeling I will need a few shifts covered. She takes care of it. I call Ted but she doesn’t answer. I text her his oxygen. I go back to a chair outside the room with Ivars and the social worker. The social worker starts saying more stuff. Ted calls. We talked and she explained stuff but I don’t really remember it all now. She was way more helpful than the social worker.
Eventually they come out and tell us the intubation is done and they are going to take him up to the PICU. The social worker clarifies paediatric ICU. Honestly had that figured out already. My brain is working very efficiently at the same time as being checked out.
This is kind of where things get foggy for a bit. Over the next week Ivars and I take turns staying over night. Riley FaceTimes with us and to talk to Charlie because she’s still sick. She’s bouncing around to Nanny and Poppa’s and Uncle Adam’s and Jana’s and to Tia’s but we are trying to keep her from Uncle Adam’s because he just had his baby girl who was premature so we don’t want to chance whatever has gotten Riley sick is the same thing that’s got Charlie in the hospital. We are starting to bring belongings and leave them. We are moving in. He’s on various types of sedation. If he doesn’t have this combination he starts to wake a bit and they don’t want him pulling on the tubes. There’s ketamine, Ativan, and fentanyl. Not drugs you really feel so good about being pumped into your kid. He’s resistant to it too so the dosing had to be a little higher. He’s like me. For some reason I’m more resistant to anesthesia as well. Tests keep happening. Specialists keep coming in. Everyone asking the same things. Was he sick before, what happened the day he came in? CT scans run. Brain looks fine on CT scan so it can’t be the brain. He’s got blood in his stomach and blood in his lungs. He had a nose bleed in the ER apparently. It’s just blood from the nose bleed they determine. They check to make sure there’s no internal bleeding. Respiratory therapists are in and out of the room regularly. Trying to clear his lungs. There’s other fluid too consistent with micro aspirations. This makes sense. He’s been choking every time he drinks. We told the pediatrician she told us to tell the OT. The OT told us to use small straws but it was still happening. I had read and aspiration pneumonia when we had taken him to the hospital a few weeks earlier because I was getting worried. They keep working to get the fluid. Blood is all out. Fluid keeps building. Ted’s working the next few shifts. Ted comes in every day. She pays close attention to his vitals. Watches what everyone is doing. She tells us what’s normal. She tells us every time that the staff that she knows are all really good but you can tell when she’s really excited about someone. Some definitely advocated more or just went the extra mile. Not a single person was bad though. One time one nurse I didn’t like at first I thought she was bossy and not overly kind to her coworkers. I texted Ted because I had seen the routines enough times that I wasn’t sure I felt good about her. I was afraid her attitude was bringing down the rest of the team. Ted reassured me that she can be tough sometimes and a little intimidating but that she’d been doing the job for so long that he was still in incredible hands. She’s tough because she cares about her patients. Sure enough we found this person to be amazing too. When it came time to be gentle she was gentle. And she got shit done. Another nurse came in for a night shift and she was amazing. We built a good relationship with her. She sat with us while we cried she explained in great detail the things we didn’t understand. She was incredibly organized and made sure that all his lines were organized. She was really thorough and tidy and just an overall person that we trusted. Then they moved her to another patient but she checked in every shift.
They still don’t have answers. Things just don’t make any sense. They’ve ruled out infection. It’s not COVID, infectious diseases has been in and ruled out any rare infections. His body isn’t getting any better and they don’t know why. He’s getting less stable. His lungs are struggling more. They haven’t done an MRI but his CT scan was good so they aren’t really worried about that. They wanted to do one just in case but he wasn’t stable enough to come off support and they couldn’t take all the supports into the MRI so they need to get him stable. It seems to be something with the lungs so the MRI isn’t a priority. The brain looked good in the CT scan so it can’t be that. So many X-rays, CT scan of his heart, heart is great. Fluid in lungs had improved but there is still some and it’s low so they can’t get it out with chest physio. He won’t cough. His blood pressure is sky rocketing. He is starting to run a fever. They switch him to a different sedation. They can’t figure out the cause of the fever because he doesn’t have an infection. Acetaminophen isn’t even touching it. We tell them he always needed Tylenol and Advil to manage fevers and Riley usually did too. They can’t do the Advil because they don’t want to risk internal bleeding into the lungs. He kept desating (his oxygen dropping) so they had to keep pumping the support up. He’d make progress and they’d start dropping it down and he’d desat again.
By the Monday morning things weren’t looking great. I was starting to tell people I knew I was losing my baby. I could feel it. He was gone already. He wasn’t coming home. This is where that nurse pushed things. Charlie was no longer waking up or responsive. Even coming off the sedation. This nurse was convinced something neurological was going on. She’s seen it before. She insisted he get an EEG and a full day one and that the MRI needs to happen. There’s an old MRI machine that they can take him in with all the support. She gets him a cooling blanket to get his temperature down. She advocates for us being able to hold him as she thinks it is good for helping him getting better. As the day goes on they are able to take him off his BP meds, temperature starts to get under control. He’s having bowel movements and peeing. No more desats. She comes in again for the next night. She starts sharing stories of her experiences of people waking up and remembering things etc. She is really comforting now and optimistic. She makes sure the team knows to let us hold him after the EEG is done.
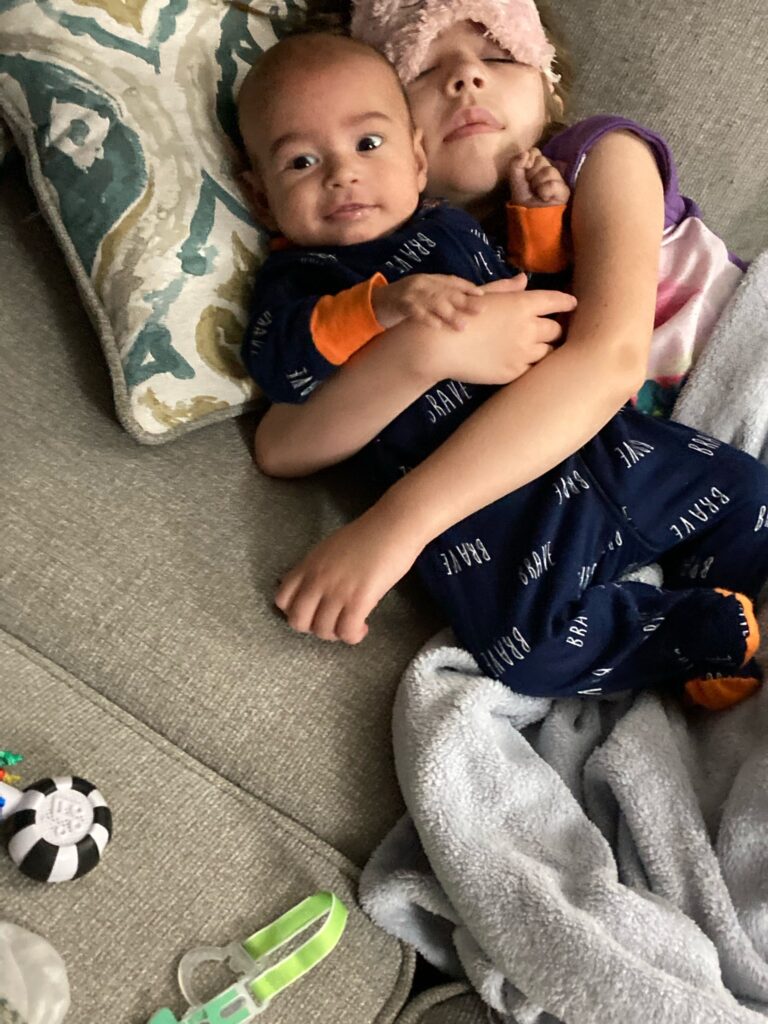
Riley and Ivars had signed up for a Daddy daughter dance class that was supposed to start that night. We felt it was important to try to keep Riley in a routine and having quality time so they went. But while they were there it was just too hard to focus. They decided after to drop the class. Riley hadn’t been to the hospital yet. She’d seen Charlie on FaceTime and read and sang and talked to him but not in person. She wanted to come that night. So she did. It wasn’t good. (Although it was in the long run) She got really upset because she didn’t realize he was as bad as he was and she refused to go home. Eventually we got her settled and she went home but then she had stomach issues from the anxiety.


The MRI was scheduled for 3:30 on the Tuesday. Charlie had some desats again and his temperature was still struggling. At this point the Genetic and Metabolics department is involved. Dr. Tarnopolsky the head of Neuromuscular and Neurometabolics comes in. He reviews the information with us. He has a theory. We showed him videos. He’s confident by the sound of Charlie’s breathing and by how rapidly things are changing and what he saw on the MRI so far it’s a condition called Leigh’s Disease. He can’t confirm it yet as the neurologist needs to review the MRI and there is more tests still outstanding but he feels pretty confident. He said once they do those tests and the MRI results are reviewed formally he will give us more details on the outlook. He seems optimistic. Ivars asks the name again and he spells it out for him and Ivars begins to Google it. He says not to get lost in the Google world because it leads to more questions. It’s too late. Ivars already did when he spelled it out. The brief description Google gives says that it’s fatal and usually happens by the time a child is 2-3 years old and the death is usually caused by a respiratory event. We are devastated and mad that the doctor even told us his theory before confirming. I can’t stop crying. Doctors come in and nurses come in to reassure us that there is still so much more testing to be done. In the evening they let me hold him. The other nurse we adored who got moved to another patient, had advocated for Charlie to be moved from a crib to a bed so we could lay with him and sleep next to him. Like when he was first born that skin to skin time to help him get better the time laying next to his family can help too. So while I held him they switched things around and I got to sleep next to him that night.
Wednesday, March 29th (the day we brought him in) Wednesday April 5th and Monday, April 10th are three dates I won’t forget. Wednesday April 5th, Charlie continues to struggle. Temperature struggles and he’s still not waking up. They have a “family meeting” for us booked with doctors at 5:30 to go over results and next steps. Father Dave and Bishop Crosby come around 3:00 for a visit. Cardinal Roche is praying for Charlie too. I’m still distraught and angry with God and scared but now comforted knowing all the support he’s getting. The Bishop anoints Charlie too with prayers for healing. As he finishes Charlie opens his eyes so briefly. I jump to him and shout he opened his eyes. The bishop says “he did I saw it!”. “Charlie baby, I’m here! Mommy’s here! Hi my baby!” He moves his hand. We tell the nurses. There’s excitement and curiosity for sure and they warn us it could be reflex but it was a really positive sign.
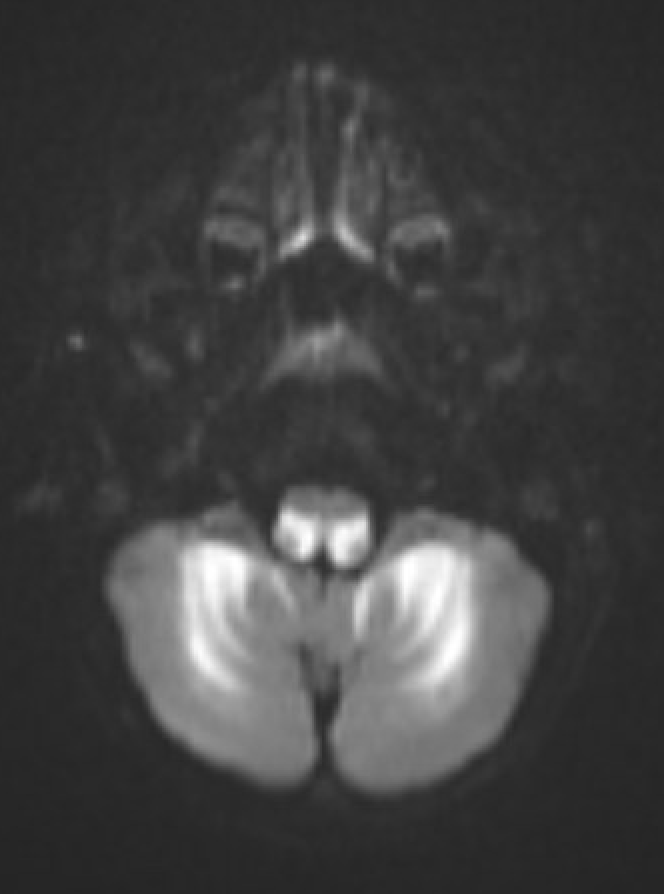
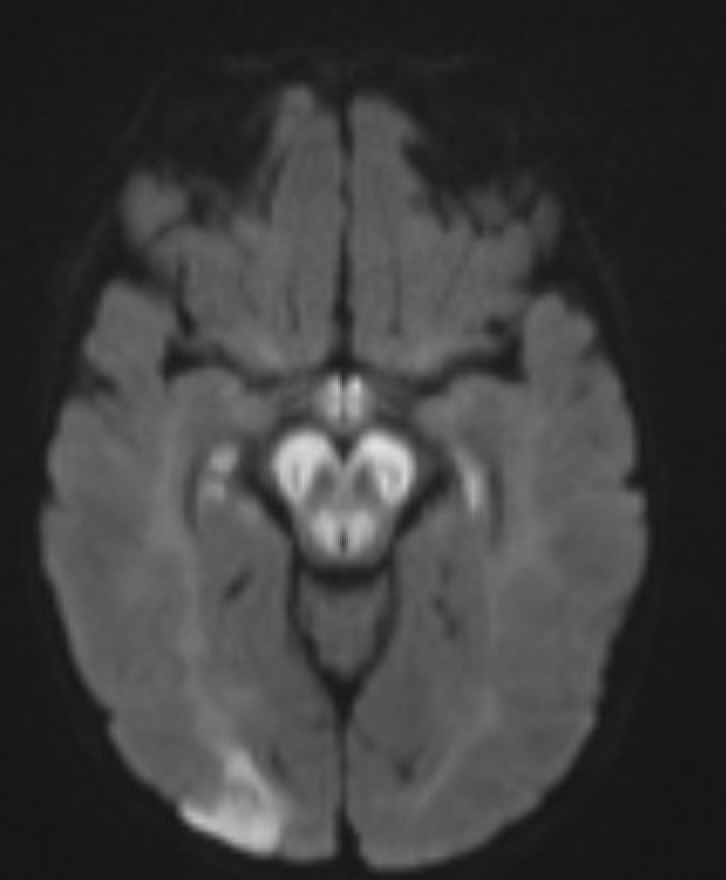
We have the family meeting. My parents had come by to visit so they stayed with Charlie while Ivars and I met with the team of specialists. They basically said all their tests had come back and the MRI results and the progression of Charlie’s state supported Dr. Tarnopolsky’s theory. Basically his brain was covered in lesions particularly around the brain stem. The part of the brain responsible for temperature regulation, lung function, heart function, swallowing, speech etc. The most likely answer was Leigh’s Disease. There was a possibility of 15 other mitochondrial diseases or one metabolic disease. None as likely though as Leigh’s. They were going to run blood work for these diseases but it would take weeks for results. Dr. Tarnopolsky though had a lab that could turn the tests around a little quicker than average so he’d use them. In the mean time treatment was the same regardless. A course of steroids would be started. In the next 4-5 days we’d know if it was working. If not it was just further confirmation. We asked what the best case scenario was for Charlie. He lives his life on a feeding tube and oxygen support. Okay we will do what it takes and what he needs. My gut though already knew from day one what was happening. I tried to be positive and hopeful and Ivars did too. They asked us if we wanted to see the MRI’s and we said yes. There was no denying the damage on his brain.
These are two of the many images they showed us. The bright white areas are areas of damage.
Riley was staying with my brother after school. We talked to the Child Life Specialist about how to share this information with Riley. We agreed to do it with the support of the specialist on Thursday. In the mean time I had to keep myself together enough to not scare her. Our dance family had prepared some meals and done some grocery shopping. So Kelly and Cat met me at Adam’s house before I picked up Riley and loaded our car. I saw them and fell apart. Riley was watching from the window. Ivars had already texted Adam and Adam pulled Riley away while I cried to Cat and Kelly. I felt my legs go weak and the two of them just held me as I faced the reality. We moved behind the cars away from the window as I told them the news and gained my composure and eventually said goodbye. Riley and I headed home and grabbed dinner along the way. At home Riley said to me “at my birthday Charlie is going to be my special guest. He gets to have a special seat at the table”. I couldn’t breathe. I died a little inside. I started crying “hopefully he’s better by then I said”. The next morning I ran around the house grabbing his toys and things for him to hold and play with. They said it might help if he starts waking up to feel the different things and for us to help him move things around. He would be starting physiotherapy. I started getting really upset because I couldn’t find Cory Carson. I became hyper focused on finding it and mad. Eventually Riley stops me and tells me Charlie needs me more than Cory.
We get there and the Child Life Specialist helps us explain to Riley what is happening to Charlie’s brain and what that part is responsible for. They let her know we are going to try some treatment to see if it will help him. Riley takes some time to watch TV and snuggle with Charlie and nap in bed next to him. Later she says she wants to hold him. So the team gets her set up to hold him. As I’m watching though I can see it in her face. The fear, the heart break, the anxiety. Charlie is limp when they lift him. He’s heavier than he’s supposed to be. They get him on her lap but I can see she wants away. I asked her if she’s okay she’s not. So they give him to me. She breaks down and spends time with the Child life specialist. They take her to different activity rooms and a sensory room to help her pull together her feelings. They have her make Charlie a hug scarf. They trace around her upper body so that it wraps around him like she’s hugging him. Eventually she comes back to be with him.They have her pick out a quilt that was donated to make the bed more comfortable for him and for him to take home if he goes home. In the evening Ivars and Riley head home. They do some chest physio and while they are doing it Charlie sleepily opens his eyes a bit. He does it a few times. They get him into my arms his eyes opening as they pass him to me. I hold him for a long time. Later that night I’m laying next to him and I roll over a bit onto his arm. He pushes me away. The nurse is seeing responsiveness and we are getting hopeful and excited. It’s not just muscle twitches its intentional movements. Overnight an RT Angie (Angela – the name of Ivars mom) comes in she gets more physio happening and is able to drop Charlie’s oxygen support significantly. They are starting to find the amount of pressure he needs to breathe is going down because it seems like he’s starting to breathe on his own a little more.









The NJADS family tells us they’ve been getting cash donations now to help with meals so they put it on Uber gift cards. When we see how much they’ve been getting we ask that perhaps the rest be put aside. If Charlie gets to come home a lot of accommodations are going to need to be made and we will probably need to take time off work etc. With the amount of support coming they decide to set up the GoFundMe.
The next few days we spend watching and waiting. Riley continues to come for the days and spend time next to him and with the Child Life team doing activities for Easter. When the days become too much she goes to see family- spending time with Tia, or at the circus with Uncle Imants. When she’s there she’s doing things to help. Learning his physio and helping with it etc. Ivars and I help with baths. His oxygen requirements are up and down. His X-rays show his lungs still have fluid and the left one keeps collapsing. His responsiveness is waning now. Nights are stressful because they seem to be when things happen.
Saturday night gets very scary. His breathing is bad and the RT is working so hard. I can see it in his eyes he’s trying so hard to keep Charlie going. He’s sniffling a lot. He looks sad. He spends a lot of time outside the room watching. I’m texting Ivars scared this might be it. Asking the team if I need to get him here to say goodbye. They tell me not yet but their eyes and body language say soon. The RT gets the Ventolin going and it helps for a while. But by the morning Charlie is needing so much support.
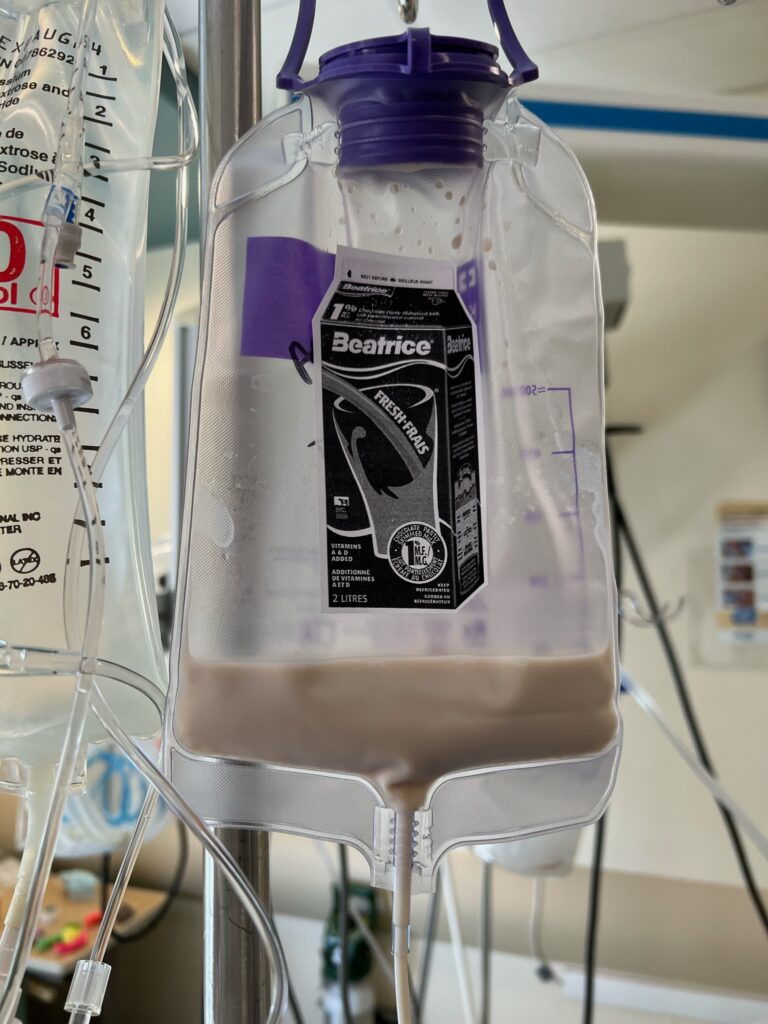
It’s Easter Sunday things are a bit calmer. We woke up to some gifts from the staff including his footprints painted like carrots and framed. Riley wanted him to have chocolate pediasure in his feeding tube because he loved chocolate milk and she hoped the Easter Bunny would bring him chocolate pediasure. They made a fun surprise for her too. The Easter bunny visited at home and we had Easter gifts from the NJADS family.






As the day goes on they can not get Charlie’s left lung recovering.In the afternoon we were noticing when we tickled his feet he moved and pulled his legs up and tensed his arms we were really excited but the doctors weren’t so much. Eventually the doctor explains that it was reflex and Charlie actually had no mental control over it. He was now not responding as well either.
THIS NEXT PART MIGHT BE HARD TO READ SO PLEASE BE PREPARED AS IT DETAILS OUR FINAL DAY. CLICK HERE TO SKIP TO DIAGNOSIS DETAILS.
It’s my night to go home Ivars gets really anxious about me going home. He has a bad feeling. Riley and I go home and she wants to set up her telescope. She wants to find a shooting start to wish on. Ivars starts texting me. Charlie and desatted again and the RT is fighting again. They can’t seem to help him. Do I need to come back? we are back and forth texting as he tells me they got it under control but then it happens again. They are going to get him on his stomach to see if that gets out the fluid. They might be able to do a procedure to get into the lung and get stuff out but they need to try this first. Things are looking bad. Ivars needs me down there. I called my parents. My mom stayed with Riley and my dad drove me because now I was too scared to drive. We sit and watch over and over as they try to intervene. They start getting fluid out. It’s reddish again tinged with blood. There’s a lot coming but the lung isn’t working. Eventually they get real with us. They can’t do anything more. He’s too weak and unwell for the procedure and we are going to have to say our goodbyes. In the morning we will have two choices. They can slowly decrease his supports and turn off alarms or they can take him off all the tubes completely and let us hold him until he goes on his own. We call home and Riley says goodbye over the phone. Not long after my parents call. Riley wants to be there with him. So they all come down and say goodbye. We sing. We read stories and cuddle together as a family. Just like we did the day he first came home. I ask my parents to take a picture. The hospital staff give us a key to a family room across the hall and Riley and I sleep there while Ivars sleeps in the room. Mom and dad go home. In the morning the doctor reviews the options again. We opt for the slow decrease in support. I start feeling sick. We continue reading and singing and talking and watching Bluey and cuddling. Charlie’s oxygen keeps going off and they have to keep coming in to adjust his oxygen. Ivars takes Riley for a walk. Anxiety gets bad and I can’t handle watching him suffer I start to get faint and nauseous and things get blurry. I haven’t had a panic attack like that in years. Our nurse isn’t around. I stumble to the desk. “I need help” “what do you need” “nurse, social worker, somebody I’m having a panic attack” and she jumps up and says okay. I get myself to the bed in the room and all of a sudden the resident doctor, the nurse and the social worker are there. Things are blurry. The doctors hands are cold and it helps. I need to go to the other room. I need ice water. I’m going to throw up. Ivars and Riley come in as they are escorting me out. The social worker sits in the room with me. I text my parents to come. She tries to offer support but says something I hate “In my religion God only gives us what we can handle” – nope. That’s it. Not going to work. No one can handle this. And even if they could that doesn’t mean they deserve it. I’m freaking out now and I’m saying how crappy I am for not being in there right now with my baby. I’m supposed to be supporting my family. As I’m saying this Riley comes in. Riley sits with me and tells me I don’t have to support them all myself. We do it together we are only strong enough together. This starts to help. My parents come back and the social worker leaves and mom comforts me enough to get out of the room. I was supposed to have a therapy appointment at 1:00 and my therapist came right to the hospital. I told her what was happening. She used to work in a hospital with end of life patients. I tell her I’m confused about the oxygen and kind of how this is playing out. She tells me I need to talk more wiht the doctors and have a very serious conversation about what is best for Charlie. She points out we always have chosen what was best for Charlie. I come back and we all talk. We are all struggling watching and waiting. Ted and I had been texting as well and she told me this could go on for days. We meet with the head doctor. She explains that the gradual decrease is really benefiting us more than Charlie because it gives us more time for our goodbyes. She tells us though that what will likely happen as they continue to decrease is that Charlie’s heart will eventually give out and he will go into cardiac arrest and they won’t be able to give him meds or anything to help prevent suffering. He will keep going through these oxygen dips and needing the intervention. She said it could happen so quick too when it does that if someone went to the bathroom he could be gone by the time they get back. His brain is no longer controlling his lungs and is far too damaged.







They explained by removing the tubes they could provide him with morphine and make sure he’s comfortable and let his body decide when it’s ready. She told us that would probably be pretty quick because all his vitals say he’s ready. She said keeping him on the tubes this point was fighting what was natural. If we went that route we could hold him until he was ready and he’d be comfortable and look more like himself and he’d be safe. We took time to talk about it and my dad told me how my grandma had been on her way home when his sister died and she couldn’t be there with her. We agreed that this was what was best for him. We told Riley. She was ready too. She wanted to be with him when he went. They gave him meds and while we waited we packed our belongings. There was so much to go home. My dad loaded it all up in the car. When the meds kicked in they eventually pulled over the bed/couch next to his bed and the three of us sat on it. They disconnected him and sat him in our laps. Ivars wanted one last family picture with out Charlie on tubes. we actually don’t have any family pictures of the 4 of us other than the day we brought him home and ones with Santa. My dad took our picture then he and my mom stood with us. Charlies eyes fluttered. He shifted or stretched. But I know it wasn’t really a stretch. Then we felt it. He had left. we held him for while and the doctor came in. She lifted his arm. I saw the colour change. She confirmed he was gone and we cried and held him a bit more. Riley had to step away. Eventually we let him go and they put him back on his bed and we said goodbye. The nausea kicked in again. They got me tons of ice cubes and a puke bag for the ride home. That bag sat in my purse for the last two months because I still get struck. The ride home was awful.
Over the last two months as we waited for results and learned more about Leighs we learned a lot of Charlie’s life was a miracle. You may have read all the previous things about how we realized now many things that were side effects of the damage. His fatigue, his loss of words etc. but that he had a better life not knowing.
After meeting with the doctor last week he confirmed Leighs. Charlie’s aspirations were due to the inability to swallow properly, his loss of words and inability to walk independently were all part of it. In his final days the fever that wouldn’t go away. One day he was so cold they had him under heated blankets and with us snuggled up to him to keep him warm. One of the earlier signs is vomiting and diarrhea which he never had however in the final days he did have loose stool which we thought could have been from being on a fluid diet but may have been because of the loss of function.
There are different ways of inheriting it but Charlie got it through recessive genes.
The genetic tests basically found that Charlie had 2 partially deleted genes in his DNA, because of that it impacted his mitochondria and this is why Leigh’s had developed. Usually it’s just an alteration in the gene and they are looking for “a spelling mistake” so it didn’t show Leigh’s at first but Dr. Tarnopolsky insisted they keep looking and they did a different test which found the deleted genes so it wasn’t found how they expected to find it. He said had it been another lab they may not have found it because very few labs specialize in this kind of thing.
They would like Ivars and I to both get genetic tests done as it’s more than likely we are both carriers since Charlie had both genes affected. Because the gene is recessive, we’re not affected by it, but there’s a 25% chance that our children can be. The fact that we would both have it, that’s incredibly rare. We won’t see results for at least 4 weeks after they get blood samples from us.
He also confirmed as well that Riley is unaffected and has no chance of suffering the same fate. This is due to multiple factors such as age and lack of any signs or symptoms. However, if Riley were to have children some day, it’s advised that she get genetic testing at the time to rule out any possibilities as she could be a carrier of the gene.
Once confirmed that we have the genes offers will be put out to the family to get tested so our siblings etc know if their children are at risk. If they get tested with it their partners will then have the option to get tested but most likely for our family worst case scenario their kids are carriers. The likelihood that their spouses are carriers too is slim so their kids won’t go through what Charlie did. They even asked multiple times if there was anyway somewhere down the line in our ancestry our families could have crossed paths making us related because it’s so rare for two people to come together with the same genetic defect. We had to reassure them it wasn’t possible.

Leave a Reply